Cancer immunotherapy, commonly using immune checkpoint inhibitors (ICI), has revolutionized the treatment of previously hard to treat metastatic (stage four) cancer. The main difference to other treatments such as chemotherapy is that it boosts the immune system rather than impairs it. Chemotherapy tries to kill cancer cells by using medications that are toxic to cancer cells (and white blood cells and other immune cells), helping to stop the cells multiplying and growing, but this also damages the immune system. Immunotherapy boosts your immune system’s ability to fight and kill cancer cells. Unfortunately, the increased activity of the immune system can lead to immune related side effects in other body systems as the immune system starts to attack healthy cells and organs. This has a similar effect to some autoimmune conditions like rheumatoid arthritis, lupus, psoriosis, type 1 diabetes, crohn’s disease, ulcerative colitis and inflammatory bowel disease. If you already have one of these autoimmune diseases, you are more likely to have an exacerbation of your symptoms during and after immunotherapy. You are also more likely to develop new autoimmune conditions. Your oncologist needs to carefully consider if immunotherapy is appropriate for someone with an autoimmune condition or if radiation and chemotherapy are more appropriate.
Although the most common side effects of cancer immunotherapy affect the skin, gastrointestinal system, endocrine systems, liver and lungs, the muscreauloskeletal and nervous system are the next most common areas affected. The most obvious issue if you have severe immune related side effects is that you may need to stop immunotherapy allowing your cancer to continue to grow and spread. Steroids are commonly used to treat some side effects and continue immunotherapy. There is an increased risk of infection while on steroids, so sometimes, antibiotics are also required. Another possible treatment is Infliximab. This is usually used for inflammatory conditions that are autoimmune associated but it does not appear to reduce the effectiveness of immunotherapy. For skin reactions, topical creams, emollients and steroids can also be used.
Approximately 5-7% of immunotherapy patients develop inflammatory arthritis. However, a much larger 40 percent develop joint pain without any arthritic changes. Tendinitis/tenosynovitis, and polymyalgia rheumatica also commonly occur and rarely pseudogout. The onset of joint pain varies widely but most commonly starts five months into immunotherapy treatment. Pre-existing osteoarthritis may increase the risk of developing immunotherapy related inflammatory arthritis.
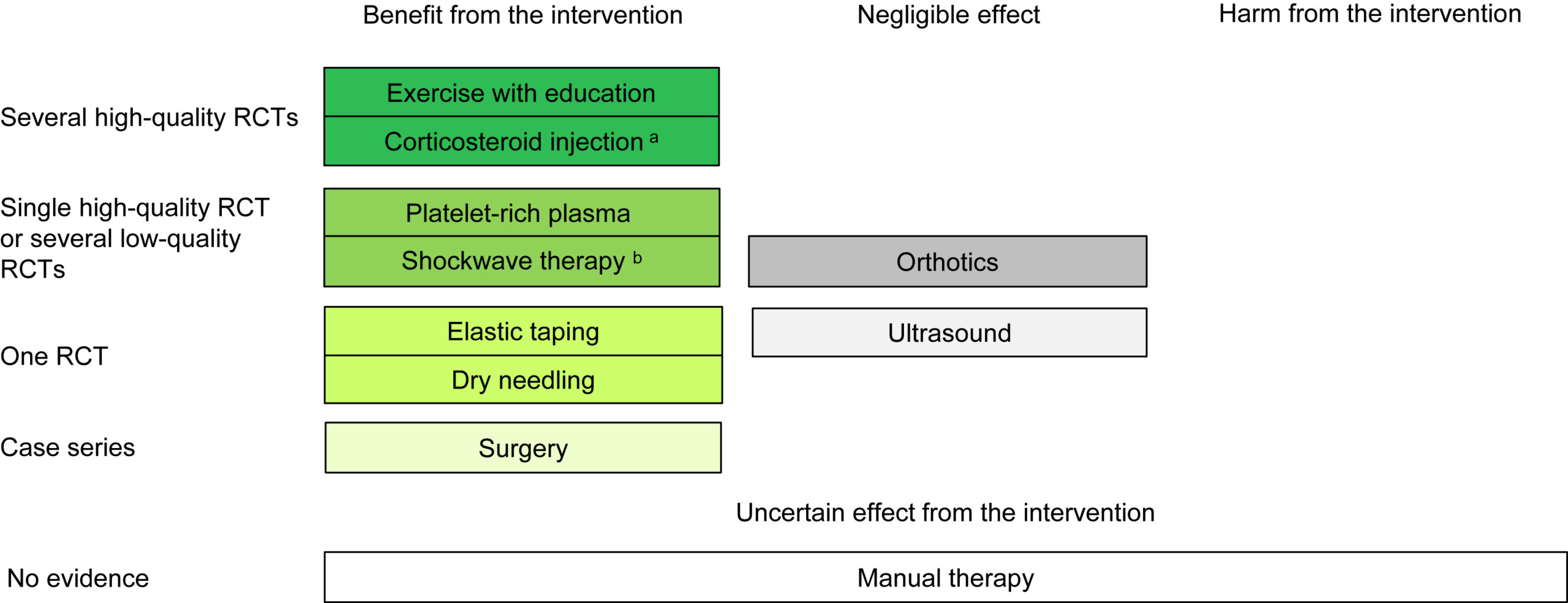
In addition to oral steroid treatment for joint inflammation, an injection of steroid into the affected joints can be useful. Severe cases may benefit from methotrexate or adalimumab, commonly used for inflammatory autoimmune diseases, and may even increase the effectiveness of immunotherapy on cancerous tumors. Physiotherapy treatments such as ultrasound, laser and manual therapy may be appropriate in some cases with oncologist guidance to alleviate symptoms.
Immunotherapy can cause neurological disorders such as peripheral neuropathies. These often appear early on during treatment and affect between 10-14% of patients. As neurological damage may cause long term disability, neurological deficits and even death, early intervention is needed. Often immunotherapy needs to be stopped and immunosuppressive treatment started such as mycophenolate, infliximab, ciclosporin, tacrolimus. and intravenous immunoglobulin.
The autonomic nervous system may also be affected causing symptoms such as fainting on standing, intestinal digestive issues (peristalsis inhibition), and difficulty sweating.
Vestibular neuritis causing vertigo and dizziness is another possible neurological side effect from immunotherapy.
The most severe musculoskeletal related side effect you can get from immunotherapy is triple M syndrome. This is thankfully quite rare at 0.1-0.3% of patients receiving immunotherapy. This condition means that you have inflammation of the heart muscle (myocarditis), muscles (myositis) and nerve-muslce endplates (myasthenia gravis). Unfortunately this can be fatal in 38-60% of patients who develop it. As the condition is so severe, it is important to check for the other M’s if you find evidence of one. Quick in hospital treatment is needed and immunotherapy needs to be stopped and immunosuppression treatment started if this develops.
References:
Cancer Immunotherapy: Managing Toxicities and Maximising Gains. Immune checkpoint inhibitor (ICI). Thu 29 Jan 2026, RSM London.
Especially: Professor Benjamin Fisher, Professor in Clinical Rheumatology, University of Birmingham. Dr Aisling Carr, Consultant Neurologist, University College London Hospital.
Yang R, Wang B, Su Z, Song Y, Zhang Y, Liu Y, Zhang Y, He C, Yang X, Zhong F, Fu Z, Ding Y, Zhang N, Li R, Chu S, Xu C, Sun J, Shen H, Geng W, Zhang S, Zheng M. Methotrexate exerts antitumor immune activity and improves the clinical efficacy of immunotherapy in patients with solid tumors. Sci Transl Med. 2025 Jun 4;17(801):eadn6921. doi: 10.1126/scitranslmed.adn6921. Epub 2025 Jun 4. PMID: 40465690.
ESMO Guidelines for Mx of toxicities from immunotherapy. Annals if oncology V33 Issue 12, 1217 1238.






Leave A Comment